Insomnia

Definition
Insomnia is the most common sleep disorder affecting millions of people as either a primary or comorbid condition. The word “insomnia’ originates from the Latin “in” (no) and “somnus” (sleep).
Insomnia is defined as a complaint of difficulty falling or staying asleep which is associated with significant distress or impairment in daytime function and occurs despite an adequate opportunity for sleep. Insomnia is viewed as a symptom and a disorder.
Characteristics
Insomnia is thought to result from a state of “hyperarousal.” As a result of this elevated state of alertness, sleep may prove difficult. Insomnia is characterized by chronic dissatisfaction with sleep quantity or quality that is associated with difficulty falling asleep, frequent night time awakenings with difficulty returning to sleep, and/or awakening earlier in the morning than desired.
At least one in three people will experience insomnia that can cause sleeplessness or waking without feeling refreshed, during their lifetime. Sleep affects all body systems and deleterious effects to the immune, cardiovascular, endocrine and neuronal systems are seen when sleep deprivation occurs (Colrain, 2011). It is important to first understand the process of sleep and the patient’s expectations.
Understanding Sleep
Sleep is a restorative physiological process characterised by an alteration in brainwave activity, viewed via an electroencephalograph (EEG). This reading shows that brainwave frequency slows as the sleeper drifts from alertness towards deep sleep (N3 phase of sleep) (Dement & Kleitman). In addition, brain, eye, skeletal muscle and heart activity change throughout differing phases of sleep, as shown through polysomnography (PSG).
Clocks and rhythms
Sleep is governed by two distinctly separate rhythms: the circadian rhythm (i.e. the intrinsic biological clock) and the homeostatic sleep drive (i.e. sleep pressure) (Borbely, 1982). The circadian rhythm is an endogenous cycle of around 24 hours, influenced by melatonin, and matched to environmental cues that synchronise the biological rhythms to the earth’s 24-hour light/dark cycle) such as light, temperature and food.
Sleep pressure is governed by adenosine levels in the pre-frontal cortex of the brain: for every hour of waking, there is a steady accumulation of adenosine, increasing the urge to sleep. During sleep, adenosine is anabolised back to adenosine triphosphate (ATP). Together, sleep pressure and the circadian rhythm form the sleep–wake cycle. Optimising factors, such as food, exercise, temperature, light and noise improve the sleep–wake cycle and are generally referred to as ‘sleep hygiene’.
The sleep–wake cycle also includes another cycle: the ultradian rhythm, which this can be depicted as a graph that shows the changes in sleep stages as in the figure below.
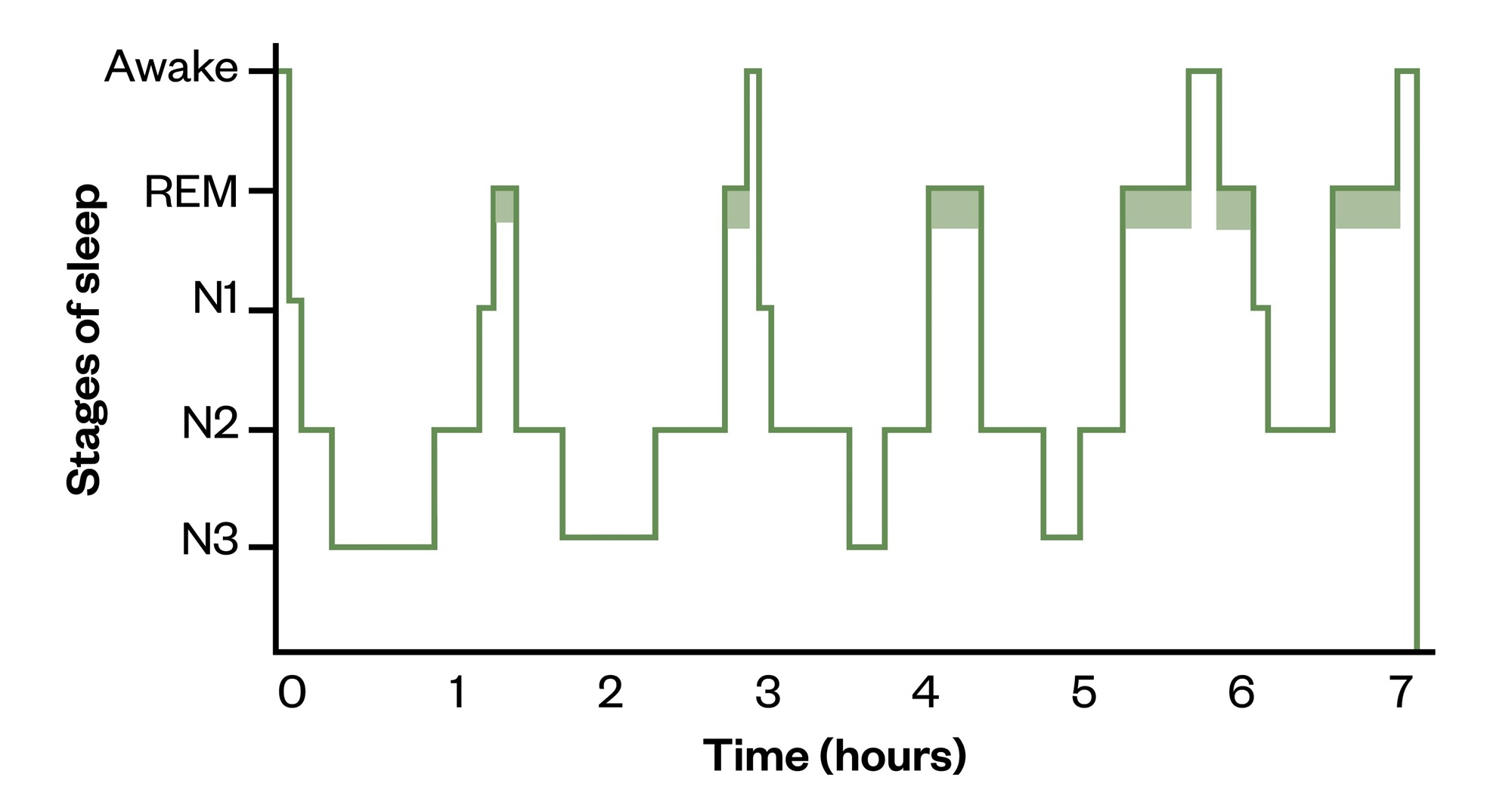
Hypnogram depicting normal adult sleep
On a hypnogram, a sleep cycle is usually around 90 minutes and there are four to six cycles of rapid eye movement (REM) sleep/non-REM sleep stages that occur during a major period of sleep. Most slow-wave sleep occurs in the first one or two cycles; this is the deepest period of sleep. The second half of the sleeping period contains most REM sleep and little or no slow-wave sleep, and may contain brief periods of wakefulness which can be recorded but are not usually perceived. The stage that occurs before waking is normally REM sleep.
Etiology of Insomnia
Diagnosis of Insomnia
The International Classification for Sleep Disorders (ICSD-3) outlines three diagnostic criteria for insomnia:
- A report of sleep initiation or maintenance problems;
- Despite adequate opportunity and circumstances to sleep;
- Resulting in daytime consequences. (Sateia, 2014)
The evaluation and diagnosis of insomnia is based on a careful clinical history of the sleep problem and relevant comorbidities. The “3-P” model is a useful framework for assessment (Spielman et al, 1987).
Predisposing factors increase the risk for developing insomnia, and include a family history and a lifelong propensity for stress-related poor sleep.
Precipitating factors are medical, environmental, or psychosocial stressors that initiate a pattern of poor sleep.
Perpetuating factors are behaviors and other factors that lead to a vicious cycle of continued sleep disturbance. For instance, many individuals with insomnia spend more time in bed trying to “catch up” on sleep. Increased time in bed and increased attention and effort to sleep fuel hyperarousal and perpetuate insomnia.
Management of Insomnia
The goals of insomnia treatment are to improve quantitative and qualitative aspects of sleep, to reduce the distress and anxiety associated with poor sleep, and to improve daytime function (Schutte et al, 2008). Insomnia treatment includes two broad categories:
Non‐pharmacological treatments and pharmacological therapies.
Non pharmacological treatments
The use of CBTI aims to reduce maintaining factors that perpetuate insomnia. CBTI is a short-term treatment that includes 4 to 8 sessions on average and adopts a multi-component approach, which typically includes sleep restriction, stimulus control, cognitive therapy, sleep hygiene, and relaxation training (Smith et al, 2003).
Sleep restriction involves limiting the amount of time spent in bed to the amount of actual total sleep time, which is typically derived from 1 to 2 weeks of sleep diary data.
In stimulus control the objective is to have the patient limit the amount of time spent awake in bed and re-associate the bed and bedroom with sleep to regulate sleep–wake schedules.
Cognitive therapy is designed to challenge maladaptive beliefs and attitudes that serve to maintain insomnia. Worrying, faulty attributions, or unrealistic expectations of sleep may lead to increased emotional distress, and thus lead to additional sleep disturbance, causing a vicious cycle. Challenging dysfunctional thoughts associated with sleep is believed to decrease the anxiety and arousal associated with insomnia. CBT helps replace dysfunctional cognitions with more adaptive, realistic, and alternative interpretations based on past evidence.
Learning relaxation techniques can be effective in reducing physiological hyperarousal in the patient. Research suggests that relaxation is especially effective in helping with sleep initiation (Morn et al, 1994)
Pharmacological treatments
Different class of drugs such as Benzodiazepines, Z-drugs, melatonin agonists, tricyclic antidepressants, orexin receptor antagonists are used.
Yogic management
Yoga Practices: IAYT based therapy module of VHG
How yogic management is different from conventional treatment?
- Yoga addresses all aspects of the human body i.e., physical, mental and emotional levels which.
- Yogic management considers removing the cause of insomnia, while modern medical approach treats insomnia as a symptom as brings in pharmacological management.
- Yoga aims at bringing a complete lifestyle modification , which acts as a common denominator for the prevention and management of insomnia.
- The conventional medical approach is known for a range of side effects including, drug dependency for sleep onset
Yoga not only aims at the quantity of sleep but also the quality of sleep.
Ayurvedic management of sleep disorders
As per Ayurveda, Nidranasha is due to aggravation of Vata Dosha (Vata Vrudhi). Remedial measures are very effective, safe and are cost effective without side effects.
You don’t need to get dependent on drugs but try these methods. The treatment for insomnia in Ayurveda focuses on:
- Improving the quality and quantity of sleep.
- Addressing the underlying cause and prevent long term health impacts due to it.
Certain herbs used are known to produce calming and relaxing effect on mind thereby inducing sound sleep. These herbs used for inducing sleep are- Brahmi , Shankhpushpi, Vacha, Sarpgandha, Ashwagandha, Jatamasi.
Therapies such as Shirodhara and Abhyanga are also very useful. They calm the mind, reduce the hyperactivity of the nervous system and improve endocrine activity.
Testimony
“I has anxiety and panic attacks. It started in the month of June 2021, during lockdown time. I visited allopathic psychologist and was given few tablets which helped for a time being. Later, after around one and half month, I decided to stop those tablets and consulted Dr. Vasudha Sharma. She advised me to take few acupuncture, Shirodhara and Abhyanga sessions along with few Ayurvedic medicines. Gradually I stopped taking allopathic tablets and felt good improvements with Ayurvedic treatments. I would recommend anyone with anxiety issues to take treatments at VHG instead of allopathy.”
– Rekha





